When people fall seriously ill from the new coronavirus, death rates become a highly personal matter. Yet we talk about them in the most impersonal of ways: with numbers.
We are told, for instance, that the case-fatality ratio from COVID-19 is 1%-2% (or is it 0.66%, or 3.28%?). And that there could be 100,000 to 240,000 COVID-19 deaths in the U.S. by mid-June, or perhaps far fewer.
I trained in medicine and now work as a philosopher of science. Over the past several years, I’ve been trying to understand how epidemiological evidence influences thinking in health care. Epidemiological data are critical in deciding public health action, such as when to ease up on social distancing.
But how should we think about the ever-shifting COVID-19 statistics as individuals and as public health decision-makers? Answering this question requires diving deeper into the meaning of the numbers.
Populations, individuals and case-fatality ratios
Epidemiological numbers like infection rates and death counts have been a grim presence in this pandemic, represented by circular tumors growing outward on maps.
The case-fatality ratio is the proportion of deaths from COVID-19 among those infected. In the three weeks leading up to April 7, the U.S. counted 11,014 COVID-19 deaths and 368,909 confirmed cases, for a case-fatality ratio of 11,014/368,909 = 3.0%.
As individuals, we have a psychological and practical need to make sense of population figures for individual lives. However, it is a mistake to conclude that your individual risk of death would be 3.0% if you were to contract COVID-19.
The factors that make one vulnerable to death from COVID-19 are distributed unevenly in the population. They are greatly underrepresented in the very young, for example, and greatly overrepresented in the very old.
The case-fatality ratio – like all epidemiological numbers – is a measure of a population, not an individual. Epidemiological numbers should inform your beliefs about your future but probably don’t reveal your “individual risk.”
Epidemiological numbers are also relative to a particular population at a particular point in time. It was recently reported in the media that a new study showed that the infection-fatality ratio for COVID-19 is 0.66%, not the 2% previously quoted. But 0.66% is the estimate for the population of China. The same study estimated the ratio in China’s population under age 60 to be 0.145%, and 3.28% in China’s population over 60.
The case-fatality ratio, like all epidemiologic figures, is neither a property of the individual nor the virus. It emerges from the interaction among a particular population, pathogen and place.
Hypothetical futures and the effectiveness of social distancing
At a somber press briefing at the end of March, the White House coronavirus team said statistical modeling had projected that there would be between 100,000 and 240,000 COVID-19 deaths in the U.S. through mid-June. That’s with the current mitigation efforts in place through April 30, including policies to promote social distancing.
The estimate was based on the results of several statistical models produced around the world, and it inherits the uncertainty of those results.
In deciding how to slow the spread of the new coronavirus, including when to ease up on social distancing, forecasters must compare hypothetical futures.
Imagine what would happen in the future if social distancing measures had never been implemented. According to models cited by the White House, 1,500,000-2,200,000 people would die from COVID-19 in the U.S.
The estimate of 100,000-240,000 COVID-19 deaths occurs in a very different hypothetical future, one in which social distancing is maintained for a few more weeks. Another model, which assumes all states use social distancing measures until June, has a lower projection of around 60,000 COVID-19 deaths by August. Dr. Anthony Fauci, who serves on the White House coronavirus task force, said Thursday that he now believes the toll will be closer to that lower number.
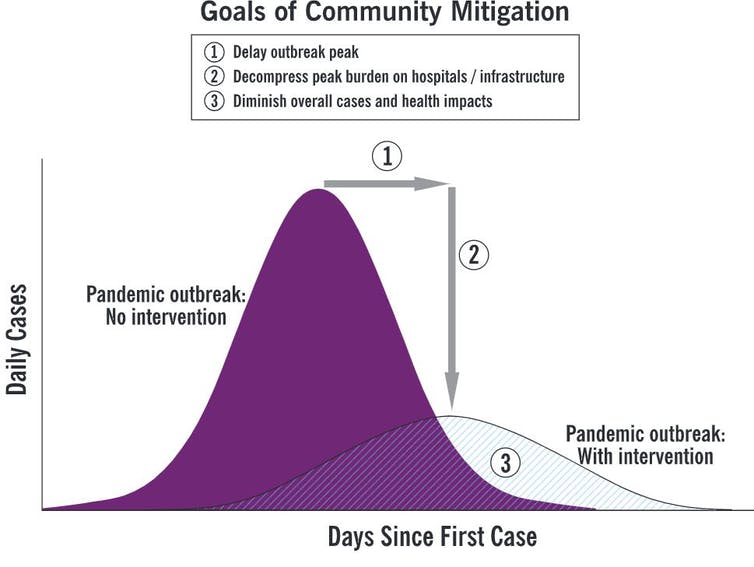
CDC
How effective will our current interventions be at saving lives? To answer that question, we compare hypothetical futures and calculate the difference in number of deaths. The answer changes depending on which futures are compared.
For example, if we compare the two futures presented by the White House, between 1,260,000 and 2,100,000 lives will be saved in the U.S. by preventing COVID-19 infections. Those numbers are why we should stay home for now and continue social distancing.
To determine when to let up on social distancing, one must similarly compare hypothetical futures. But we also must consider what else will be going on in these hypothetical worlds.
Will public health surveillance and contact tracing be scaled up? Will everyone be wearing face masks in public? The answers to these further questions will determine what will happen when social distancing measures are relaxed. As the number of modifiable variables rises, so does the number of hypothetical futures to contemplate.
Which number matters most?
In comparing deaths, outbreak modeling typically focuses only on those deaths that result from the direct physiological effects of the pathogen. However, there are other deaths to consider, due to other effects of the virus and our interventions.
A steep, unchecked rise in infections would overwhelm the health system, risking further deaths not only among patients with COVID-19 but also among other sick people who need health care.
Prolonged social distancing has economic implications, as does an uncontrolled outbreak or a secondary outbreak that might occur if social distancing measures are lifted in the wrong circumstances. An economic downturn, including job losses, has far-reaching and sometimes surprising effects on health and survival.
Another important caveat is that the effects of our interventions, like all epidemiological numbers, also depend on population and place.
When comparing higher-income countries with lower-income countries, distributions of age and diseases and patterns of social interaction and health care resources often differ substantially, which can influence the effects of COVID-19 interventions like social distancing policies. Their effectiveness can’t be simply extrapolated from one context to another.
Ultimately, deciding which effects of our interventions to measure and how to measure them is not a purely scientific problem; it is also an ethical problem. Summing deaths assigns moral worth to life and treats all lives equally. Counting life-years lost and effects on quality of life assumes that how much life is lived and how it is lived also matters. Some effects are more difficult to quantify or predict but must not be ignored, especially when we have the ability to offset them with further action.
We must think more broadly than an outbreak model thinks.
In a pandemic, numbers can tell us a lot. They speak more to us the more deeply we understand them.

